BRIDGING THE GAP
IN HEALTHCARE

Why Care Partners Medicine
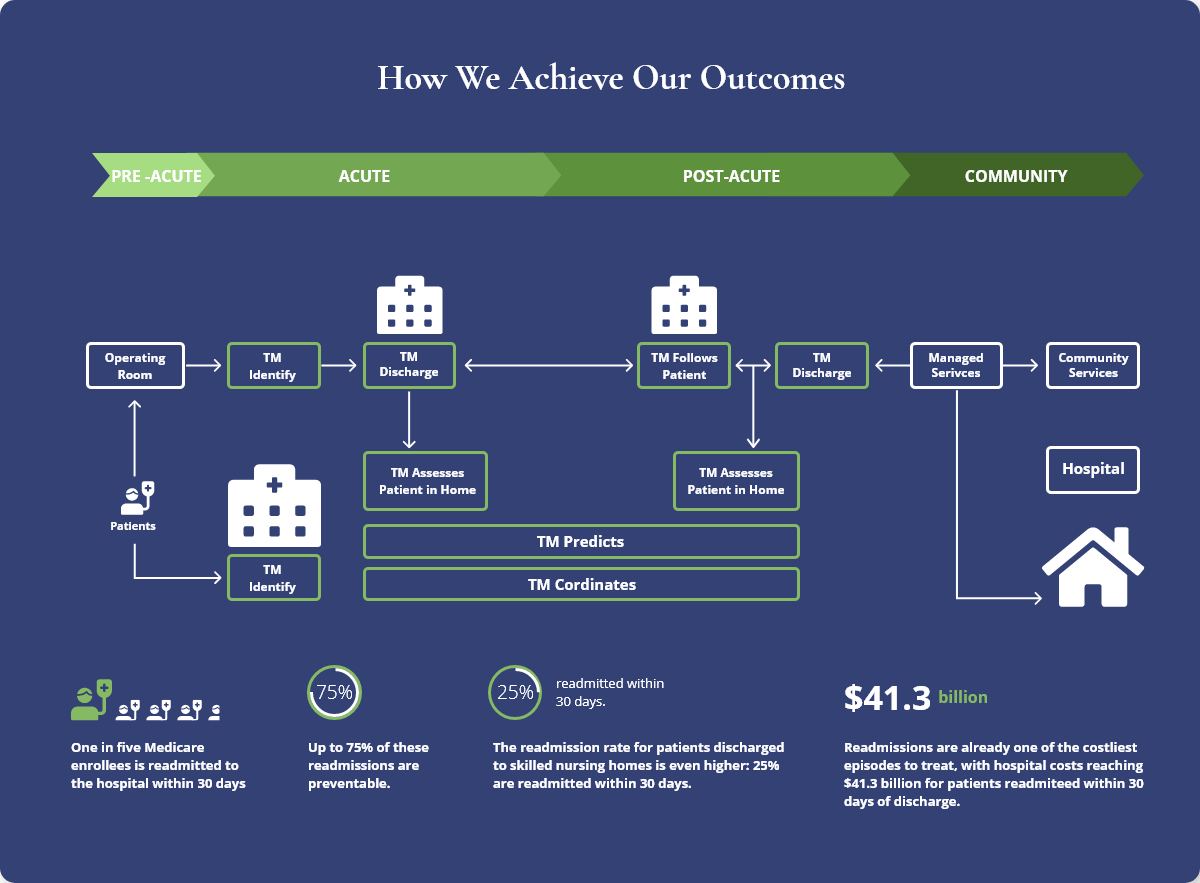
Care Partners Medicine was created for you – our patients and our healthcare partners. Focused on Transitional Medicine and Primary Care, we strive to make a difference in the changing world of medicine and medically-focused cost containment. Our belief is that care should not be about the “episode”, but rather a longitudinal look at each patient’s historical clinical utilization coupled with the patient’s care goals and social and environmental determinants that affect his/her overall health and patient journey.
We also believe that we can’t do it alone. Our model has and will always be one rooted in collaboration, communication and transparency. Our team of physicians, Nurse Practitioners and nurses excel in the homes of our patients, but also foster meaningful relationships with other post-acute partners to establish a village around each of our clients.
There is no finger-pointing on our team. Our model is stronger because our practitioners and provider partners are working together toward a collective goal: a patient-centered and personalized approach to a healthier life for each of our patients.
Caring Roots & Measurable Results
As partners and thought leaders, we aggregate and share our data and outcomes. Our goal is to educate our partners and influence the delivery of Post-Acute care. The in-depth capture and review of data allows us to be proactive in our service delivery and anticipate typical patient pitfalls prior to their occurrence.
We track and analyze the following, among various other KPIs:
- Cost Reduction and Medicare Penalty Reduction
- Patient Acuity Demographics
- Medications (# at - SOS vs EOS)
- ED Diverts
- Root Cause Analyses of successful discharges as well as any readmission
- Length of Stay
- Collaboration with Post-Acute Resources
- P4P & BPCI Improvement
- Readmissions (Preventable, Non-Preventable, All-Cause, By Bundle, By Dx, etc.)
- Clinical Interventions
Who We Partner With
Care Partners seeks out Hospital Systems, Medical Centers, Payers, IPAs and Post-Acute Care Providers with a shared vision of providing exceptional outcomes and an overall better quality of life for the most at risk, high-acuity patients in our healthcare system. Together, we can break the cyclical nature of acute care utilization and provide true value-based care.
Hospital Systems
Commercial Payers
IPAs
Post-Acute Care Providers
In addition to the above, our partners rely on us for:
- Reduction in unnecessary Emergency Department visits and subsequent admissions
- Reduction of Readmissions, costs and associated Medicare penalties
- Reduction in Length of Stay
- Improvement of HCAHPS Scores, Star Ratings and other patient satisfaction ratings
- Improvement of performance within Collaborative Care Networks (CCNs)
- Improvement within BPCI and P4P Initiatives
We help our partners deliver exceptional patient outcomes while breaking the cycle of acute care utilization for the highest-risk patients.
Readmissions for patients of this acuity are typically between 30-40% and we’ve consistently improved this to ~6% for our partners.
These patients are also the ones who most greatly affect healthcare systems’ BPCI and P4P initiatives as well as tip the scale on penalizable readmissions for Medicare.
It Takes a Village. And We Are That Village.
Care Partners provides the most robust Transitional Care Platform in the market.

Care Partners’ Patient-Centered Approach
The foundation for our model centers around Dr. Mary Naylor’s Clinical Approach to post-acute Transitional Medicine. Accordingly, at Care Partners Transitional Medicine, Nurse Practitioners with a specialization in Post-Acute Care carry the laboring oar for our service delivery. Our NPs visit frequently with our patients in the home setting and are supported telephonically by a team of Transitional Medicine RNs, LVNs and Coordinators.
As we evolved, it became apparent that that we needed to further address the psychosocial factors which were increasingly relevant in achieving long-term patient success. In that vein, we incorporated aspects of Dr. Eric Coleman’s Social Work-driven “Transitions of Care” model to create a hybrid transitional care model which puts the uniqueness of each patient at the forefront of our services.
Because health and recovery are not just about clinical or episodic factors relative to a patient’s most recent admission, we believe building a relationship and treating the whole patient is critical in breaking the chain of cyclical acute care utilization. Taking this kind of approach allows us to view the patient outside of the episode that led to his or her most recent admission. Even more, as successful treatment often involves more than simply clinical support, our practitioners openly communicate with our patients to understand any underlying personal motivators or treatment goals.
Even with the above, we can’t do it alone. In almost 100% of cases, we are working alongside home health, physical or occupational therapy, home care and various other Post-Acute Care Providers. We’re thankful for the collaboration we receive and believe that the best care takes a village!
Be First AND Be Better
Care Partners Transitional Medicine was the first Medicare-approved medical practice specializing exclusively in Transitional Medicine in the nation.
Care Partners' All Cause Readmission Rate
Care Partners' "Preventable" Readmission Rate
Over 65% of our patients are characterized as "high risk for readmission", with an average age of ~82 and an average medication count of >13 at the start of service.
37.12%
Average Readmission Rate for Patients of comparable acuity WITHOUT Transitional Medicine Services
Our Average LACE score is 12.1. The average 30-day readmission for patients with a LACE score of 12-15 is 37.12%.
*Per UC Irvine Health Study of 3,184 Patients with LACE score of 12-15.

We Make Things Personal
>10times
Connects with
our patients
1-1.5hrs
Avg. time spent

The average time spent by our NPs with the patient during an in-home visit is consistently between 1 – 1.5 hours. The reason for that is to provide a thorough medication reconciliation and assessment of all clinical and psychosocial factors that could affect the likelihood of successful treatment.
We Make Things Personal
The results are in. More time with patients equals better patient outcomes.
>10times
Connects with
our patients
1-1.5hrs
The average
time spent
The average time spent by our NPs with the patient during an in-home visit is consistently between 1 – 1.5 hours. The reason for that is to provide a thorough medication reconciliation and assessment of all clinical and psychosocial factors that could affect the likelihood of successful treatment.
We know transitional medicine necessitates substantial patient contact. That’s why, on average, we connect with our patients >10 times throughout the average 30-day length of service.
Speed Matters
Post-discharge success comes down to acting carefully but quickly. At Care Partners, we believe that reducing readmissions starts the minute our patient leaves the hospital. Most readmissions occur within 48-72 hours of discharge. For that reason, we strive to connect with our patients within 24 hours of discharge and are in the home within 48 hours. This allows us to ensure compliance with discharge instructions and prescriptively intervene, as necessary.