Optimize Transitions of Care

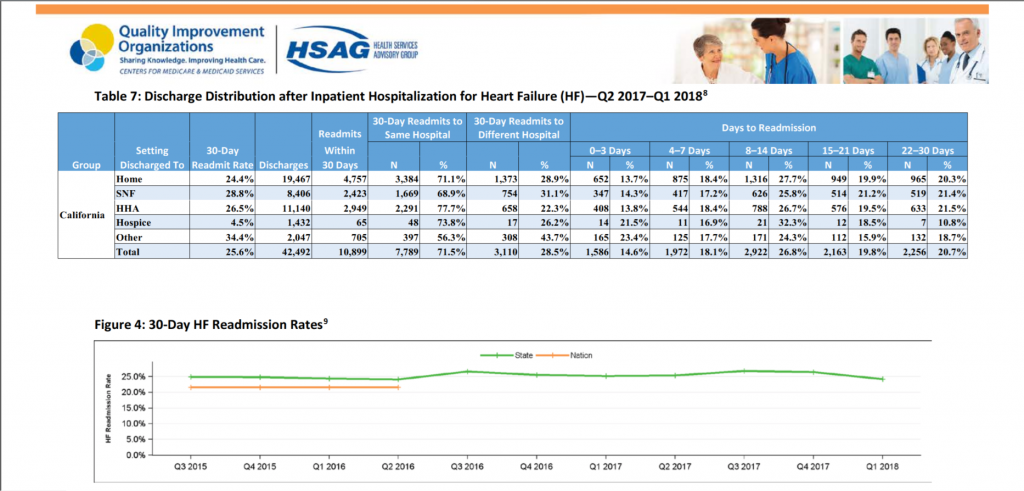
Looking at the HSAG data, California hospitals continue to struggle with readmissions within their Heart Failure patient population. Below is an excerpt from an article titled, 3 Strategies to Reduce Hospital Readmission Rates, Costs. Care Partners Transitional Medicine was built from the mold of the Coleman model and our current CHF readmission rates over the course of 2018 & 2019 are <5%.
Strategy 2 – Optimize Transitions of Care
“Ineffective care transitions following a hospitalization increase the rates and costs of hospital readmissions. Inadequate care coordination, such as lackluster care transition management, accounted for $25 to $45 billion in wasteful spending in 2011, Health Affairs reported.
Communication breakdowns drive ineffective care transitions from the hospital to post-acute care or home settings, the Joint Commission explained. Technological and cultural barriers prevent providers from sharing information among themselves and caregivers.
The commission also pointed to accountability breakdowns as a contributor to poor care transitions.
“In many cases, there is no physician or clinical entity that takes responsibility to assure that the patient’s health care is coordinated across various settings and among different providers,” the commission wrote. “Providers – especially when multiple specialists are involved – often fail to coordinate care or communicate effectively, which creates confusion for the patient and those responsible for transitioning the care of the patient to the next setting or provider. Primary care providers are sometimes not identified by name, and there is limited discharge planning and risk assessment.” The accountability challenge causes patients and other providers to receive insufficient knowledge and resources for at-home or post-acute care.
To overcome communication and accountability challenges, hospitals have used “transition coaches” who are primarily nurses and social workers to help create and guide post-discharge care. These coaches are usually the single point of care for patients.
A model widely used by hospitals is the Care Transitions Program. Eric Coleman, MD, MPH, developed a program that uses a nurse or nurse practitioner as a transition coach to manage post-discharge care.”
Site Source: https://revcycleintelligence.com/news/3-strategies-to-reduce-hospital-readmission-rates-costs